The parotid gland produces saliva, that juicy substance that makes your mouth water when you're about to bite into a savory double bacon cheeseburger (or for you vegans out there, a juicy portabella, roasted poblano pepper and tomato burger, slathered with refried black beans and grilled onions--as a devoted carnivore, I found this surprisingly satisfying) and is one of the three major salivary glands found in the face and neck. Surgery on the parotid gland is often done for tumors. Most tumors (neoplasms) of the parotid gland
are benign (non life-threatening); approximately 80% are benign leaving a 20%
chance of malignant tumors. One of the
most common benign tumors—called a pleomorphic adenoma or benign mixed
tumor—however, carries a small risk of converting to a malignant tumor later if
it is not removed.
Usually a needle biopsy is done, if possible, to render a
diagnosis. Benign tumors often are
removed since they can become quite disfiguring if left to grow, and removal
may be more difficult the larger they become. The facial
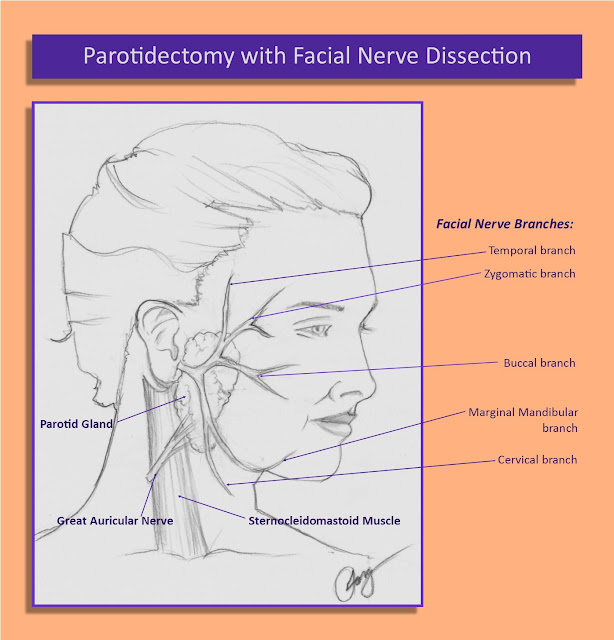
nerve is within the substance of the gland and divides into its various
branches inside the gland. A simple
excision of a parotid mass is not possible without damaging or cutting the
nerve. Also, most tumors require removal
of a sizeable amount of normal tissue around the tumor; otherwise small
vestiges of tumor can be left behind and it can recur later down the line, and
operating in a site that had prior surgery is more difficult.
Thus, if you have a parotid tumor and your doctor feels it
needs to be removed, then the surgery is a parotidectomy
with facial nerve dissection.
Oftentimes an explanation of the surgery goes a long way in
preparing the patient for surgery and the postop after-effects. This article provides a basic description of
the surgical approach.
First of all, the surgical incision is placed in way that is
has the most cosmetic after-appearance while providing wide exposure. The often the Modified Blair incision is
often used.
Next, a flap of skin and the fatty soft tissue beneath
is elevated off the fascia or capsule of the gland and this is retracted forward
(anteriorly).
There is a nerve that enters the gland from below called the great auricular nerve, which provides sensation
to the lower face and lower part of the ear. Since it enters and branches within the
gland, saving this nerve in majority of cases is not possible, and thus it is
cut. I tell patients to expect this, and
they will notice a permanent numbness along those areas the nerve serves,
namely the lower face and lower part of the ear.
Next, the dissection goes deeper, peeling the gland off the
sternocleidomastoid muscle, the front part of the mastoid bone and the front
part of the ear known as the tragal cartilage, and more gentler dissection is
done to identify the facial nerve. This nerve must be preserved in all cases,
unless there is direct involvement with tumor (in such cases facial weakness is
often present before surgery). The facial nerve is responsible for movement of
the facial muscles on that side, including: raising the eyebrow (temporal branch);
closing the eyelid (zygomatic branch); raising the upper lip and nasolabial fold,
which is the fold of the skin from the edge of the nose that extends to the side
of the corner of the lips (buccal branch); movement of the lower lip and chin
(marginal mandibular branch); tightening the layer of platysma muscle along the
side of the neck (cervical branch).
Once the main trunk of the nerve is identified, each individual
branch is located while the part of the parotid gland over it is released. Often the tumor is in this superficial lobe. Imagine a plane with the facial nerve and
its branches. The part of the gland outside
(or lateral) to this plane is called the superficial
lobe, and the gland deep to this plane is called the deep lobe. Once each branch is followed out to the
end of the gland, the superficial lobe is attached only to Stensen’s duct that enters
deeper into the soft tissue and into the mouth; this duct is then cut and the
entire superficial lobe with the tumor is removed. If the tumor is in the remaining deep lobe, then the facial nerve above
this is gently dissected of this part of the gland, and the deep lobe is then
carefully removed.
Afterwards a drain is placed, the wound is closed with
absorbable sutures deep to the skin and removable sutures over it, and many-times
a pressure dressing is applied over the surgical site. Dressing and drain is
removed the following day in the majority of cases.
Pain needing prescription pain medications usually lasts for
a week or less, and many patients have taken plain Tylenol instead. The incision is kept dry. I usually recommend placing an antibacterial
ointment such as Neosporin, bacitracin or triple antibiotic ointment over the
suture line before and after bathing or showering for the first week. If removable sutures are placed, they are
usually removed within seven days.
©Randall S. Fong, M.D.


Comments
Post a Comment