 |
| Figure 1 |
Here's some fun stuff--surgery for the DIYer. That was meant as a joke. Seriously though, you shouldn't do this yourself or any self-surgery because unpleasant things such as pain and uncontrollable bleeding can occur leading to even more unpleasant things such as panic and death. The last post (TheDeviated Nasal Septum, June 24, 2018) described the anatomy of the nasal septum. Sometimes surgery is required to fix a deviated septum, called a nasal septoplasty, often referred to simply as “septoplasty,” where the suffix -plasty is medical lingo meaning “to mold or shape.”
The prior post described some of the problems related to a deviated
septum, but the main indication is for nasal obstruction—that is, difficulty
breathing from the nose. I usually
recommend surgery based on how bothersome this is for the patient and if it
significantly affects his/her quality of life.
The Procedure:
This often is a fun surgery and usually under general
anesthesia since the sound of scraping and bone crunching inside one’s head is
kind of unsettling, to say the least. And
so the majority of patients want to be “out completely, and don’t wake me up
until it’s all done.” After the patient
is asleep, cotton pledgets with a dilute cocaine solution are placed inside the
nose. Yes, the same cocaine people snort
for recreational purposes, but the medical form is much less concentrated and
unfortunately won’t make you high. Too
bad. Cocaine however has a dual purpose:
it anesthetizes or numbs the inside of the nose but also decongests the
tissues, meaning the mucosal tissues shrink down. This allows better visualization and
significantly reduces bleeding, as cocaine vasoconstricts (narrows) small blood
vessels. For surgery such as this, it’s
a wonderful drug, and if used properly has little in the way of adverse side
effects.
Anyway, don’t decided upon surgery just so you can get a
little hit of cocaine, ‘cause you won’t experience what you’d think you’d
experience if you were using the powdered, street stuff which is much stronger and also illegal, if you hadn’t known.
Keep yourself and your doctor out of trouble and don’t request a gallon
of cocaine for your surgery (it only comes in little bottles and is diluted to
a 4% strength).
After the cocaine is allowed to do its thing, lidocaine with
epinephrine is injected deep to the mucosa and along the cartilage and bone of
the septum. This acts the same way as
cocaine, allowing for additional numbing and vasoconstriction, but serves
another cool purpose, creating an avascular plane, which allows for later
lifting and separating of the soft tissue from the underlying cartilage and
bone.
An incision is made along the front (anterior) part of the mucosa
covering the cartilage and a plane of dissection is identified (see Figure 1 at
the top). The mucosa is that moist pink
tissue lining the inside of the nose (as well as the mouth, throat, etc) and
secretes fluid and mucous to keep the inner nose moist. Deep to the mucosa is a tough fibrous layer
called the perichondrium, which is
tightly adherent to the underlying cartilage.
This layer along with the overlying mucosa is collectively called the mucoperichondrium. Once this plane is identified, it separates readily
in most cases (unless there was prior trauma or prior surgery and thus dense
scar tissue is encountered); this is made easier with the prior injection of lidocaine
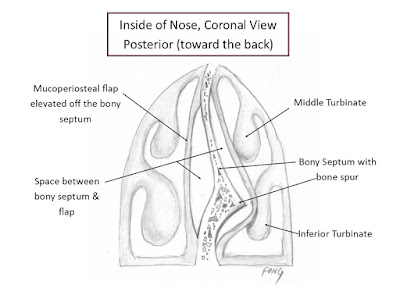
and epinephrine into this plane (Figure 2). Figure 2 (and Figure 3 that follows) is a coronal view, or a slice through the frontal plane of the inner nose. Notice the septum is deviated to the left and the mucoperichondrial flap is elevated off the right side of the septum.
 |
| Figure 2 |
This mucoperichondrial flap is then elevated from front to
back (from anterior to posterior) until bone is encountered. The junction between the cartilage and bone
(known as the bony-cartilaginous junction
and the reason medical training takes a long time so that ultra-long words like
this can be said with a straight face) is then separated. Then periosteum
is encountered, which is the fibrous layer covering the bone, and mucoperiosteal flaps are elevated on
both sides of the bony septum (Figure 3).
Cool, eh? The deviated part of
the bony septum is carefully removed with a variety of different
instruments. Since the bone of the
septum for the most part sits more posteriorly, it does not provide structural
support to the external nose, and thus as much bone as needed can be removed.
 |
| Figure 3 |
Once the required bone removal is done, the cartilage is
allowed to swing back to the midline, much like a door hinged from above. As much cartilage is preserved as possible,
since it is more anteriorly and provides support to the external nose and contributes
to some aspects of the shape and contour of the nose. If the cartilage is significantly bent or
curved, relaxing incisions are made on the concaved side of the cartilage in
order to relax that curvature.
Once the septum is back in the midline, the incision is
closed with an absorbable suture that usually falls out 1-2 weeks later. The opposing flaps of tissue must be
compressed together; otherwise, blood and fluid will form between them, causing
a bulging and widening of the repaired tissue, leading to nasal obstruction and
defeating the entire purpose of this surgery.
In the old days, this was accomplished by tightly packing 3 feet of
ribbon gauze on each side of the nose in a layered fashion, which was removed a
week later. Patients couldn’t breathe at
all from the nose and the pain and discomfort could be unbearable for
some. This was the worse part of the
surgery. Also, removing the gauze was
very painful. Nowadays, there are
fortunately more comfortable methods to keep pressure on the septum, usually by
means of thin plastic splints sewn through and through the septum (i.e. suture
is placed from one side through the splint, septum and splint on the opposite
side, and then passed again through the splint, septum and opposite splint and
then tied into a tight knot) to keep it tightly in place (see Figure 4). Think of the septum tightly sandwiched
between these splints and you get the picture.
As Figure 4 shows, some splints have a semi-cylindric breathing tube
that allows for better passage of air since the tissue of the nasal sidewalls
often swells after surgery and can lead
to temporary nasal congestion or blockage.
 |
| Figure 4 |
The splints are removed about a week later. The nose is first sprayed with a decongestant
and anesthetic spray to reduce discomfort.
The suture is cut and removed and the splints slide out. This is far more comfortable and quicker than
the old style packing.
After surgery (both with and later without the splints)
patients need to keep the nose moist by gently spraying both sides with a nasal
saline spray, 3 or more times a day.
Also, for about two weeks one should avoid any pressure to the nose,
avoid manipulating it, and avoid vigorous nose blowing, heavy exertion, sports
or exercise; otherwise, a severe nosebleed or disruption of the surgical repair
can occur, not to mention a good deal of pain.
Many patients use a narcotic pain medication but often stop
about 2-3 days postop (after surgery) using over-the-counter acetaminophen
(Tylenol) instead. Sometimes there is a
bit of cartilaginous memory, where a residual curve is noted of the
cartilage. This often can be massage
straighter with a cotton tipped applicator on follow-up appointments, and often
this eventually becomes straighter as further healing and natural scar tissue forms.
Though there is no bone between the opposed mucoperiosteal
flaps farther back in the nose, this tissue eventually scars and firms up with
time. A septoplasty results in a more
normal, straighter partition between the left and right nasal passages, leading
to easier nasal breathing. Hope this
helps. Now go out and smell the roses.
©Randall S. Fong, M.D.
Very interesting blog! I like to read it. Please visit my blog as well.Septoplasty Surgery in Islamabad
ReplyDeleteThanks For sharing this intrusting blog also visit my blog Septoplasty Surgery In Islamabad
ReplyDelete